High-deductible plans have shifted responsibility to patients. Your EHR doesn't surface it.
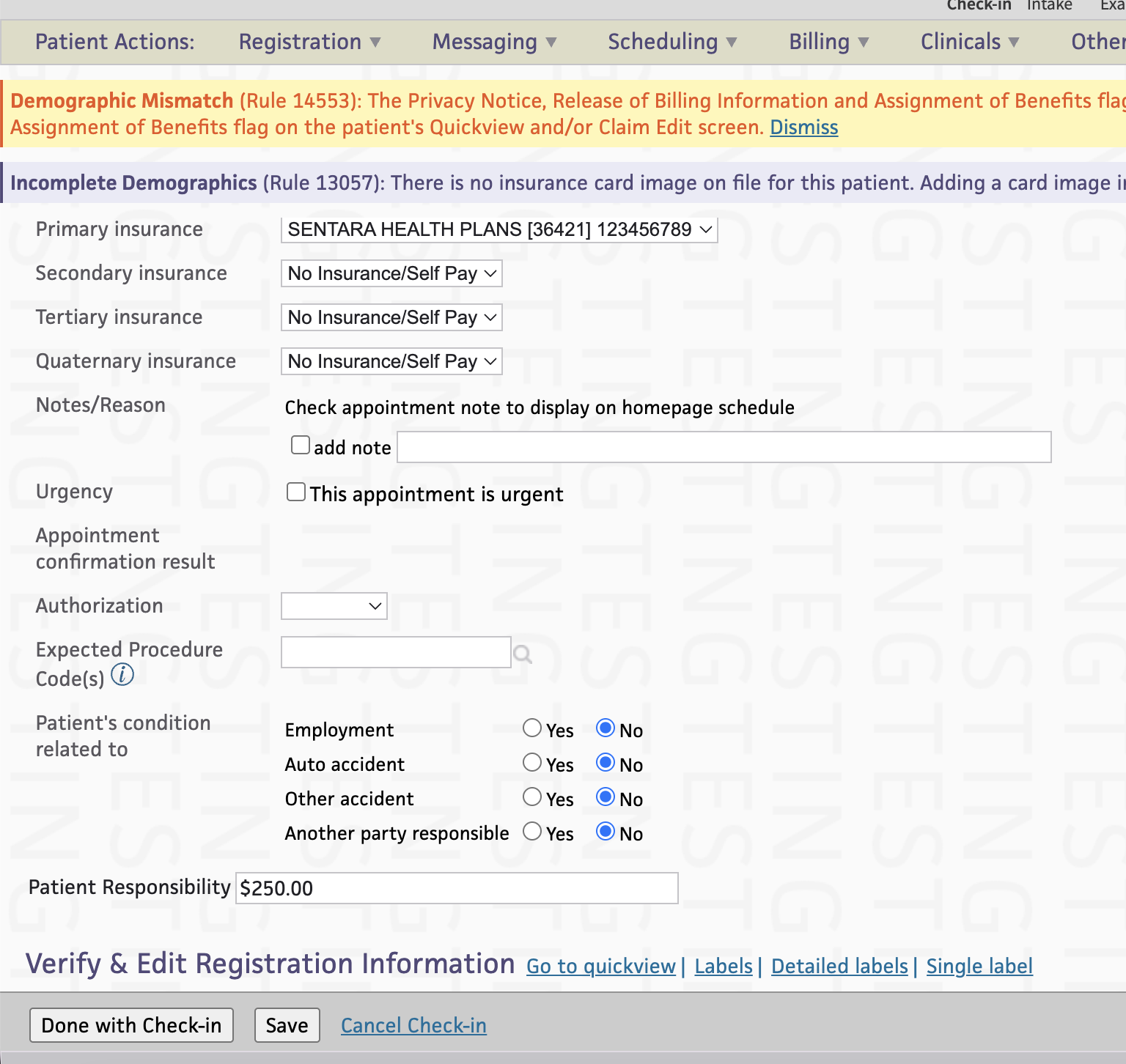
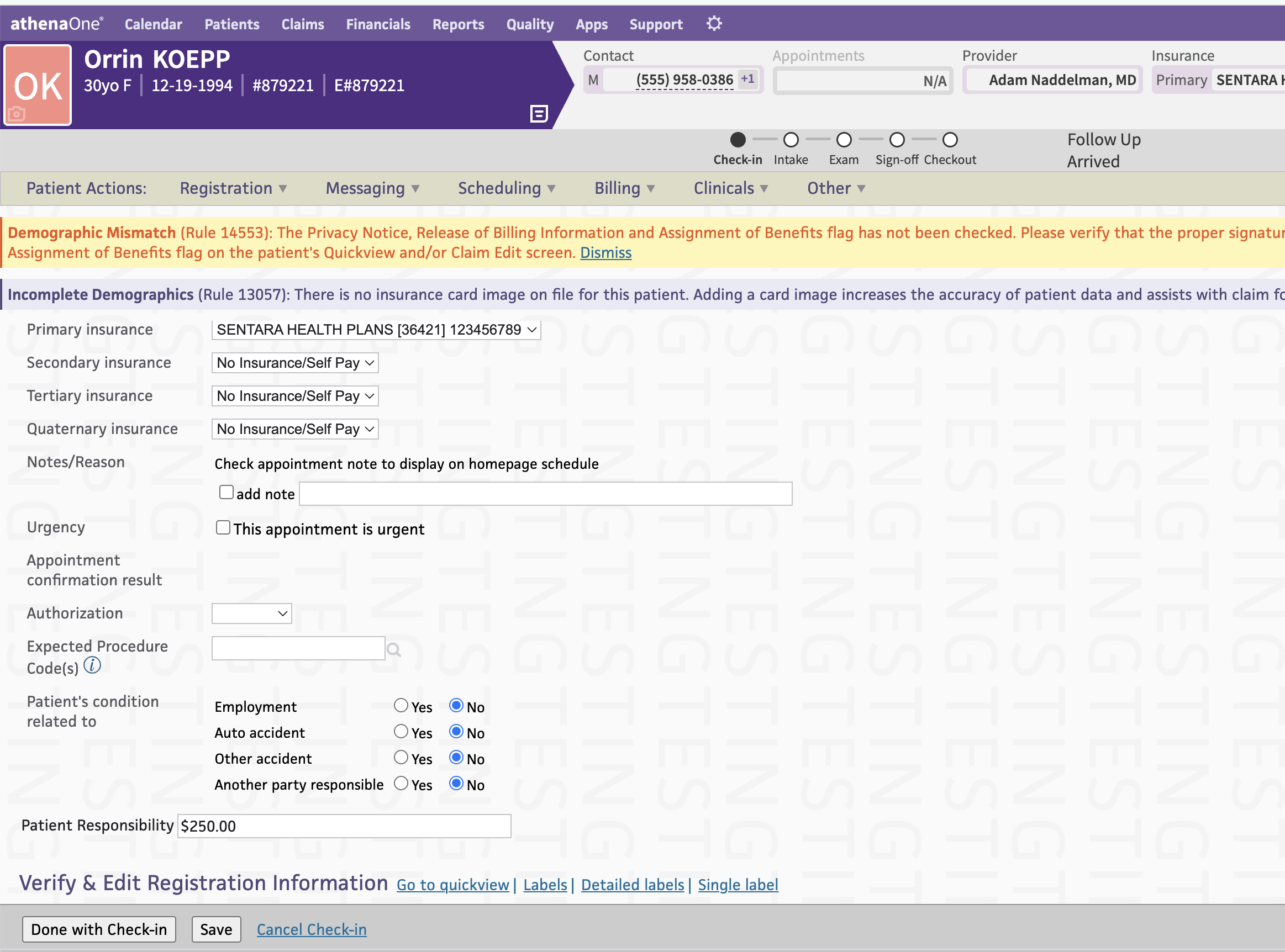
Front desks don't know what patients owe until after care is delivered — if at all.
Without clear balances, staff rely on estimates, sticky notes, or skip the conversation entirely.
Uncollected patient responsibility adds up — and chasing it later costs more than collecting it upfront.
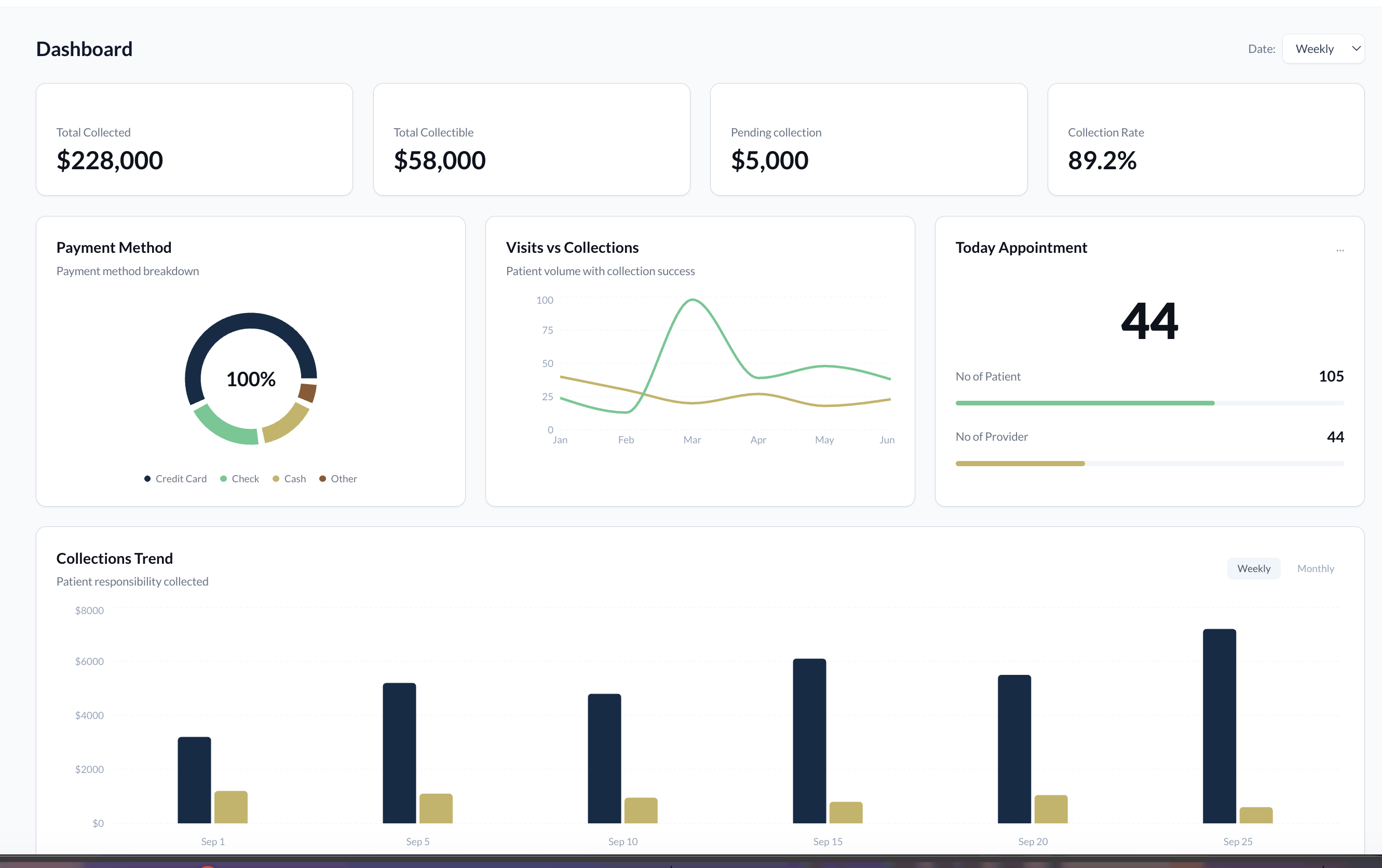
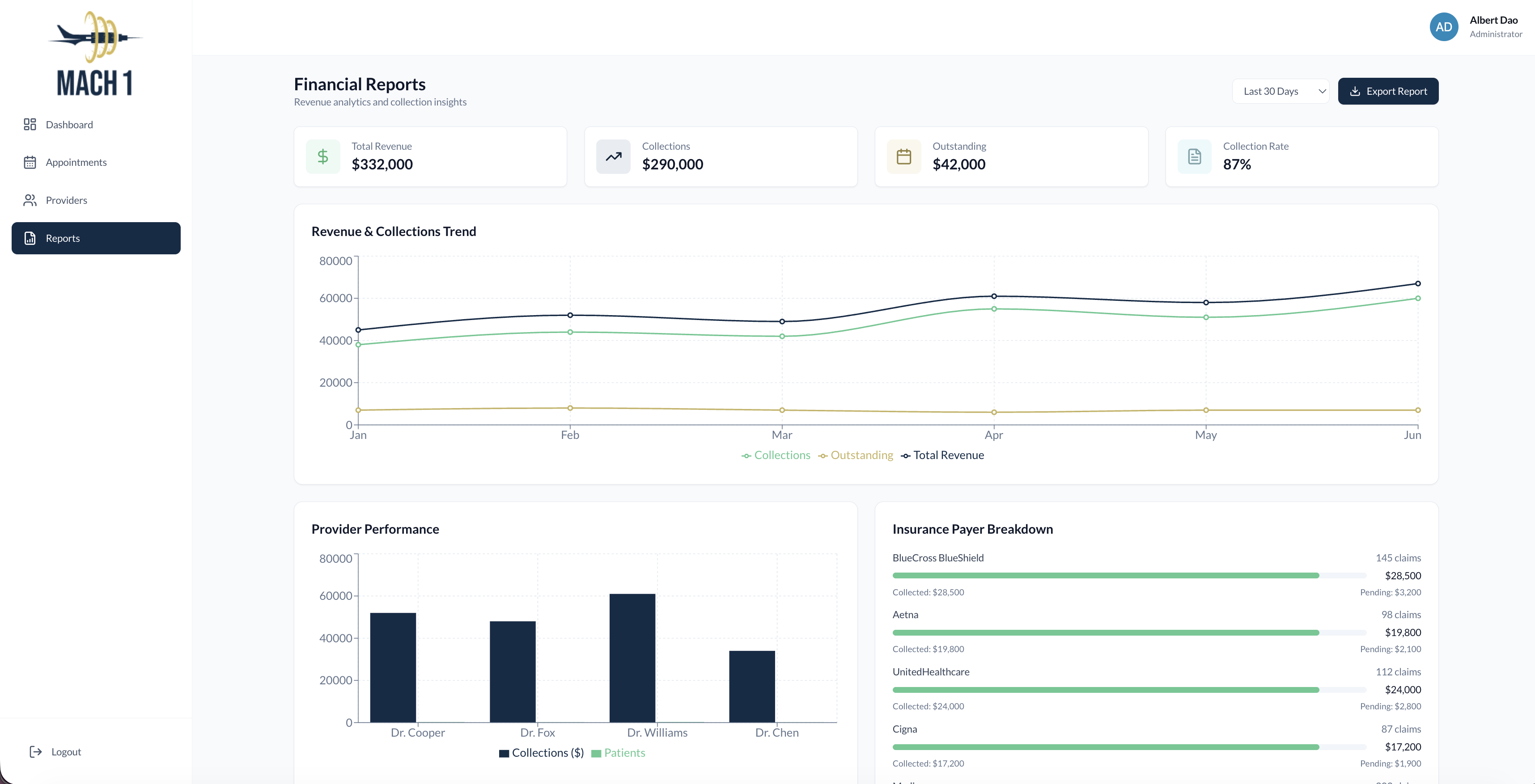
Leadership has no line of sight into collection performance, bottlenecks, or staff training needs.
Mach 1 Collections calculates patient responsibility in real time by pulling appointments, provider details, and eligibility data directly from Athenahealth. We surface clear, actionable estimates before the visit — right where your team needs them.
No new logins. No workflow disruption. Just accuracy, clarity, and faster cash flow.
We ingest appointment, payer, and eligibility data from Athenahealth automatically.
We determine patient responsibility using plan details and appointment context.
Responsibility is displayed in-context for front desk and care teams — no separate system required.
Leadership sees collection performance, trends, and coaching opportunities through an intuitive dashboard.
Know what each patient owes before care — with accuracy and confidence.
No guesswork. No sticky notes. Clear balances your team can communicate and collect.
Embedded where you already work. No separate logins, no new workflows.
Track how well your team is collecting, identify bottlenecks, and coach for measurable improvement.
We don't sell generic platforms and hope they fit. Mach 1 Collections was designed from real front desk experience — for the people who actually do the work.
See how Mach 1 Collections works with Athenahealth — schedule a live demo today.